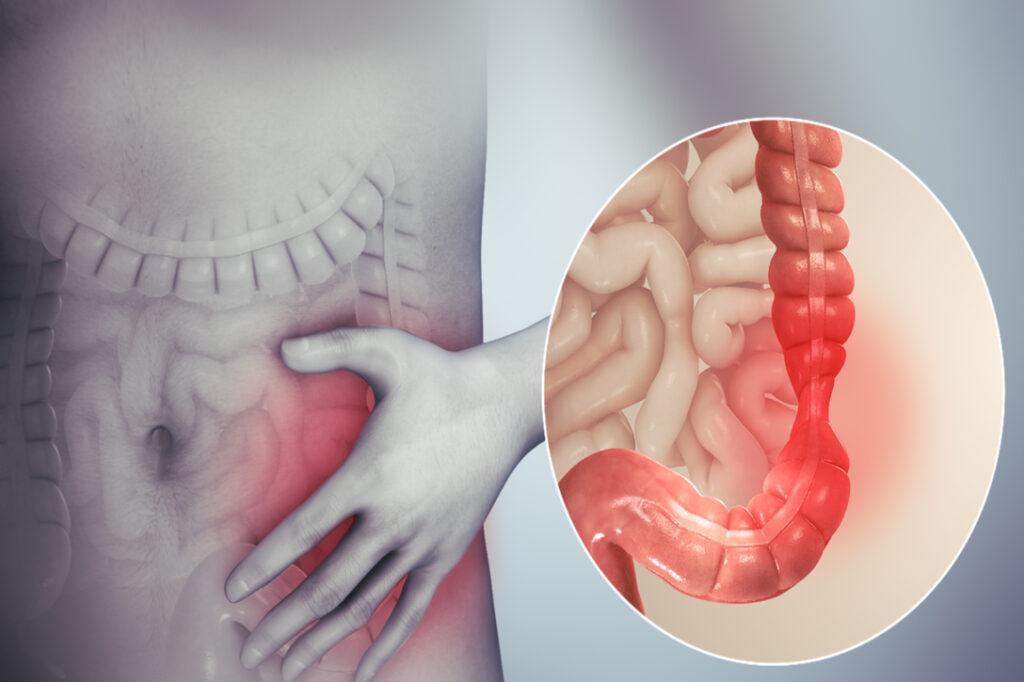
The tests came back clear. You don’t have coeliac disease and there’s no evidence of an Inflammatory Bowel Disease (IBD) such as Crohn’s disease or ulcerative colitis and by exclusion, you are diagnosed with irritable bowel syndrome (IBS). This is supposed to be good news, but after months of crippling pain and debilitating symptoms, it can be hard to see it that way.
IBS affects approx. 15-20% of the Irish population and symptoms include abdominal pain, bloating, constipation, diarrhea, and fatigue. Researchers in the APC Microbiome Institute in UCC have also discovered a higher prevalence (approx. 50%) of IBS sufferers experience anxiety and depression as the gut microbiota (the bacteria in our digestive tract) can influence our emotions.
IBS symptoms can vary from very mild in one person to severe in another and while IBS might not seem like a big deal; for sufferers, it can be extremely upsetting, embarrassing, and sometimes debilitating.
How can I get tested for IBS?
Always start with your GP as many of the symptoms of IBS can be caused by other conditions that need to be ruled out.
Research shows that an estimated 60 – 80% of IBS sufferers have Small Intestinal Bacterial Overgrowth (SIBO). Individuals with SIBO often experience severe bloating and they struggle to tolerate lots of different foods.
If a SIBO test is positive, the overgrowth can be treated and a low FODMAP diet has been shown to be beneficial to alleviate symptoms. FODMAPs are types of sugars found in a range of foods and when consumed by people with IBS, the sugars are fermented by bacteria, resulting in bloating, gas, and pain.

What can I do to reduce my IBS symptoms?
As there is not one specific cause for IBS, no one diet works for everyone. These are some general guidelines that may provide some relief.
1. We have all heard of “Eating a rainbow” but a variety of colourful fruit and vegetables will provide fibre and polyphenols which will increase the quantity and variety of beneficial bacteria in your gut. Aim for 2 fruit and 4+ vegetables per day. A probiotic supplement can also be beneficial but is not always tolerated well – speak to local independent health food for advice.
2. Dehydration can contribute to constipation and diarrhoea can contribute to dehydration. Include at least 1.5L water per day and more if you need it.
3. 80% of Irish people do not eat enough fibre which may be a major cause of constipation. Increase fibre by increasing fruit and vegetables and also, choose oats or wholegrain options of rice, pasta or bread. Sylliflor can be added to your daily routine.
4. Intolerance to certain foods such as lactose (sugar in milk), wheat or gluten (protein in some grains) or foods containing high levels of FODMAPS can also be problematic. Eliminating these for a short period of time can be beneficial to reduce your symptoms. NOTE: a low FODMAP diet eliminates a lot of ‘healthy’ foods and following a restricted diet longer term is not recommended.
5. If you are stressed, rushing and eating on the run, your poor digestive system might not get a chance to realise that food is on the way and this stress can trigger IBS symptoms. Take 5 breaths before you eat to allow your stress response to ‘switch off’ and you’re your digestive system to ‘switch on’.
IBS can be very successfully supported through diet and lifestyle. The key is identifying what is causing or contributing to the symptoms; eliminating the underlying factors and re-balancing the digestive system. When making changes, I recommend working with a qualified nutritional therapist who is experienced with IBS and will design an individualised plan just for you.